Gut-Skin Connection
When we say “gut microbiome” we are referring to all the microbes, like bacteria, fungi, protozoa, and viruses, that live on and inside the digestive tract.
Our gut microbiome is essential for digestion, nutrition, detoxification, immune function, and overall health and wellness.
The gut microbiome plays a role in whether or not other organ systems, like the skin, function the way they should. Check this out:
Gut bacteria play a role in the development of a strong, healthy immune system, especially during the first 3 years of life. If this process is interrupted, it can result in allergic conditions like eczema, and food allergies, and asthma.(1)
Levels of good gut bugs tend to be lower and levels of not-so-good ones higher in people with eczema when compared to levels in people without eczema.(1)
Colonization of the gut with C. difficile early in life can lead to eczema.(1)
Rashes like eczema are inflammatory conditions. Good gut bugs and "stuff" they produce lower inflammation, and not-so-good gut bugs produce "stuff" that increases inflammation.(2)
Short-chain fatty acids (SCFAs) are an example. They are anti-inflammatory and made by gut bugs when they ferment dietary fiber. This is why it's important to eat prebiotic foods like quinoa, sweet potatoes, and other starchy and non-starchy vegetables.
SCFAs play an important role in determining the makeup of the skin bugs you have too (we have a skin microbiome also), which then influences the immune function of the skin. When these bugs are out of balance the skin barrier can become damaged, and a damaged skin barrier is a problem with rashes like eczema.(2)
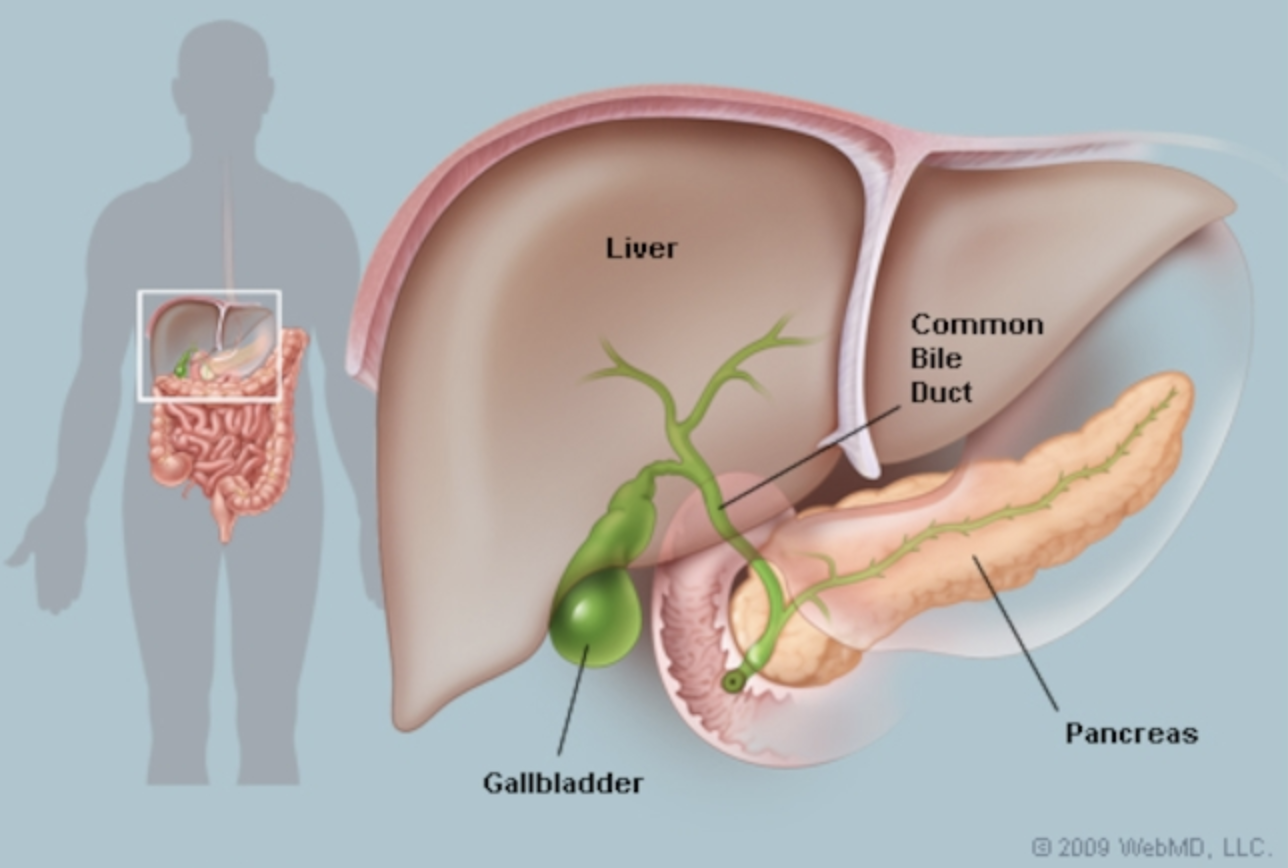
Also, in cases of leaky gut (an underlying problem with skin rashes), gut bacteria and "stuff" they produce can get out of the gut and into the bloodstream, accumulate in the skin, and disrupt your skin's healthy balance leading to rashes and rash flares.(2)
This process causes inflammation throughout the body too, triggering the immune system to go nutty, leading to inflammatory conditions like eczema.(2)
Not only does "stuff" from gut bugs get into the bloodstream, so do food particles and this is what causes food sensitivities. That's right, food sensitivities are really just another symptom of gut problems. They are a trigger for rashes, but not a root cause.
Probiotics For Chronic Skin Disease
Probiotics are live microorganisms (typically bacteria or yeast) that can provide health benefits when consumed, generally by improving or restoring the gut microbiome. Probiotics are considered generally safe but may cause problems in some people and in some cases.
Probiotic benefits include reducing skin inflammation,(3) and lessening the severity of illness and disease when taken in high enough doses.(4)
Probiotics for atopic dermatitis
The establishment of the gut microbiome early in life plays an important role in the activation of the immune system. If this process is compromised, an imbalanced immune response can result, leading to inflammation, and this can contribute to the development of eczema.(5)
Probiotics can suppress this inflammatory response.
The benefits of probiotics have been widely explored for the prevention and treatment of eczema. For example, supplementing mom with Bifidobacterium breve M-16V and Bifidobacterium longum BB536 during pregnancy, and mom and baby during the first 18 months of life may lower the incidence of eczema.(6,7)
L. rhamnosus supplementation for mom during pregnancy may lower chances of baby developing eczema for the first 11 years of life, and may protect children from developing other atopic conditions like asthma, hay fever, and allergies.(8)
Probiotics for psoriasis
Lactobacillus pentosus GMNL-77 supplementation in an animal study led to improved skin symptoms with psoriasis. This probiotic strain also suppressed inflammation associated with psoriasis.(9)
Supplementation with Bifidobacterium infantis 35624, also may decrease levels of inflammation in psoriasis.(10)
Another probiotic to show promise in psoriasis is Lactobacillus sporogenes. There was a case study on this where a woman with psoriasis that wasn’t getting improvements with typical, conventional treatments (like steroids and methotrexate) did get improvement in her skin symptoms after supplementing with this strain for 2 weeks, and then with ongoing use, symptoms continued to improve.(11)
Probiotics for acne
A small Italian study found that supplementing with a probiotic combination of Lactobacillus acidophilus and Bifidobacterium bifidum reduced acne in study participants.(12)
It has been shown that probiotic supplementation in addition to an antibiotics (like tetracycline, often used for acne) may reduce acne more than using antibiotics alone.(13)
Probiotics for rosacea
More research is needed to better understand how probiotics could support people with rosacea. There are connections between gut dysbiosis and rosacea(14), so addressing gut imbalances, including using probiotics, can be helpful.
Using Food To Support The Gut Microbiome
Probiotic Foods
Fermented foods are probiotics and they contain live active microbes. Examples are yogurt, kefir, miso, kimchi, and sauerkraut.(15) Baby and child can even have a teaspoon or so of the liquid from sauerkraut and kimchi for example.
Prebiotic Foods
Prebiotics are non-digestible components of food, like fiber, that feed gut microbes. Prebiotics can influence the activity of gut microbes, and therefore influence our health.(16)
For example, anti-inflammatory SCFAs are made by good gut bugs when they ferment prebiotics. SCFAs lower the production of toxins from gut bugs, suppress inflammatory immune responses, and increase IgA levels in the gut, which helps strengthen the immune system.(17) All of this is important to consider with skin conditions because of the gut skin connection.
While there are prebiotic supplements available like inulin,(18) arabinogalactan,(19) and guar gum,(20) a food first approach is preferred. Foods rich in prebiotics include chicory, Jerusalem artichoke, garlic,(21) onions, shallots, and spring onion, leeks, chickpeas, lentils, beans, bananas, grapefruit, almonds, flaxseed, bran, and oats.(22)
Many prebiotic-rich foods are considered fermentable FODMAP foods, thus they can contribute to gastrointestinal symptoms and maybe contraindicated in certain people for a period of time.(23) This can be the case in people that have small intestinal bacterial overgrowth (SIBO) for example.
Applying The Research In Clinical Practice
Babies and Children, versus adults
What we do in babies and children is very different from what we do in adults. Additionally, the gut microbiome changes throughout life, and certainly changes during different life stages. This is why it's important to work with a practitioner familiar with these factors rather than making a go at it on your own. No supplement is benign!
What probiotics I use most and why
Did you know the wrong probiotic can make your child’s rashes worse? True story! Certain bacteria strains, including those found in many probiotic supplements, can increase levels of histamine in the body. When your child is struggling with rashes (and food reactions), histamine is already a problem. Adding more can throw fuel on the fire and make symptoms worse. Stop guessing which probiotic to use, get my FREE Guide “The probiotic mistake you’re making that’s flaring your child’s rashes” to find out which probiotics to avoid, and which to try instead.
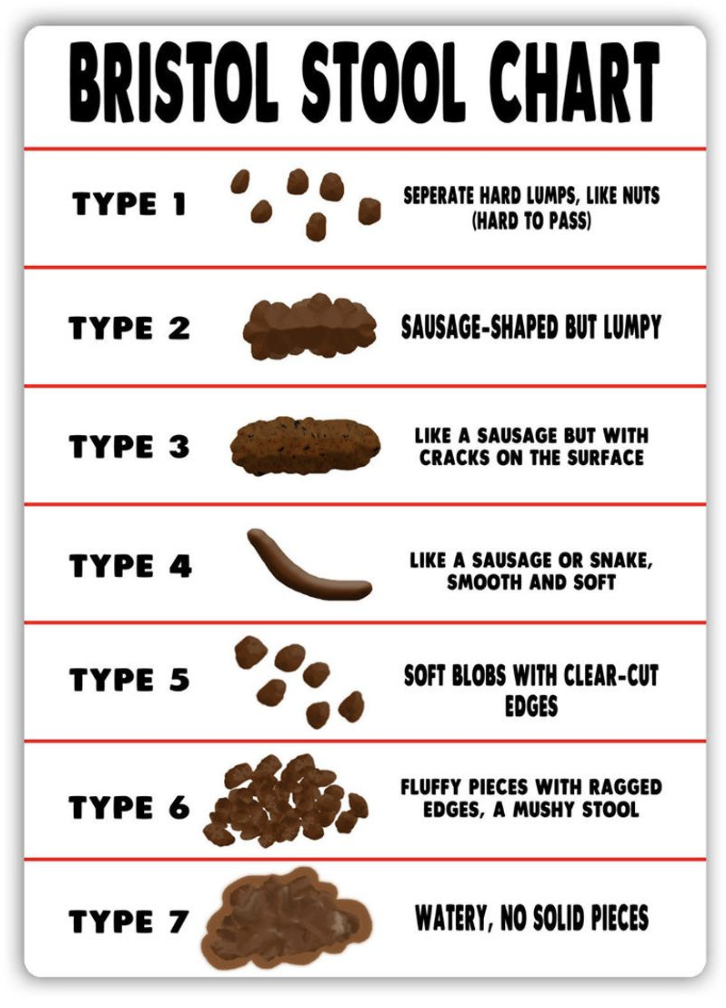
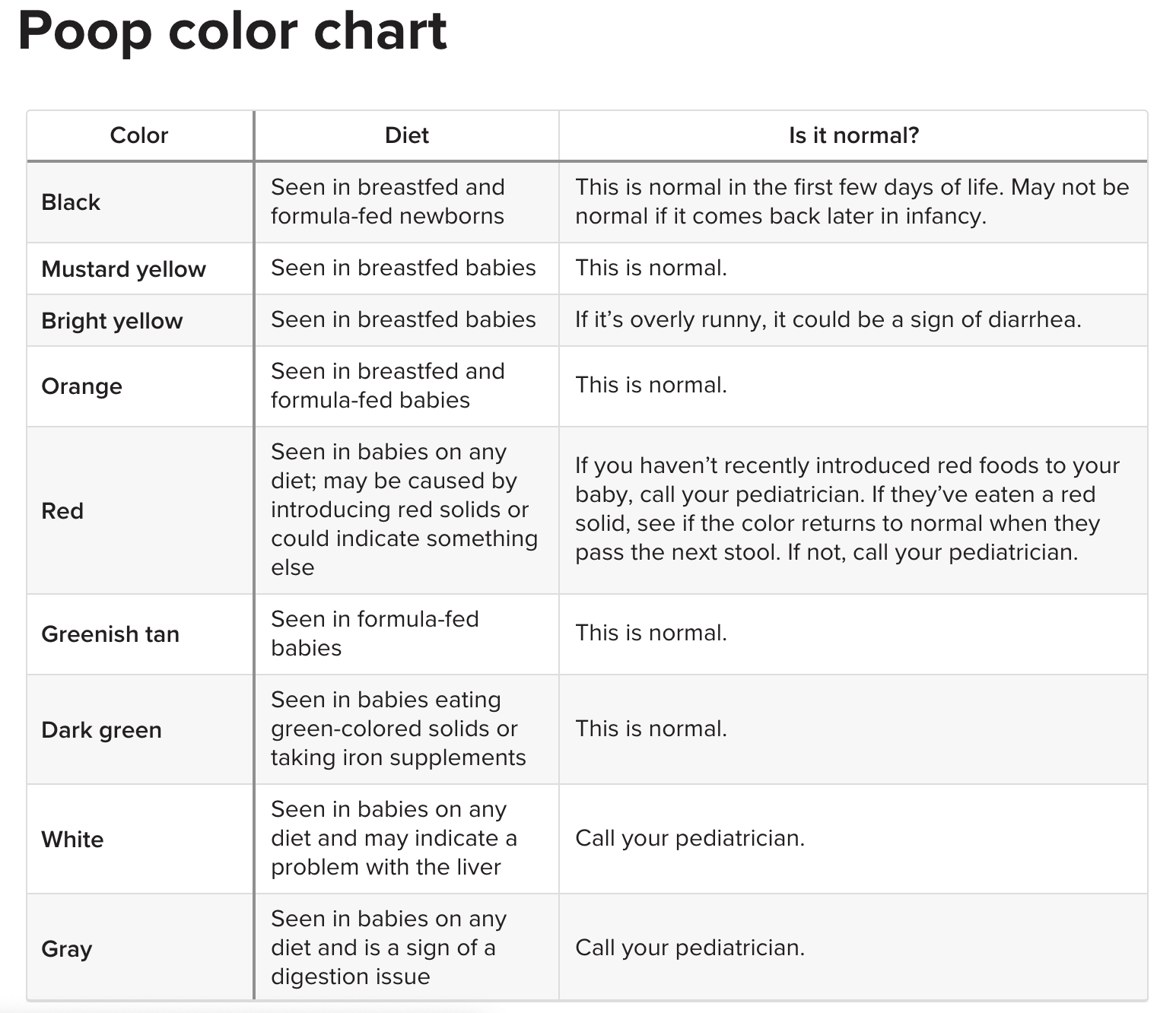
We can also dial in even more specifically which probiotic is right for your child when we use a comprehensive digestive stool test (GI Map is my go-to here) to find out what’s happening in the gut. This testing is so essential that I include it with my one-on-one services, and you can get it at a discount with Conquer Your Child’s Rashesᵀᴹ (CYCRᵀᴹ) Online.
What About prebiotics
While probiotics introduce bacteria into the gut, prebiotics feed what's already there.
Prebiotic supplements are available. Some that I use with clients include inulin,(18) arabinogalactan,(19) and guar gum.(20)
I don’t always recommend a prebiotic supplement for my clients. It's dependent on our test findings. I do always recommend eating prebiotic foods like chicory, Jerusalem artichoke, garlic,(21) onions, shallots, and spring onion, leeks, chickpeas, lentils, beans, bananas, grapefruit, almonds, flaxseed, bran, and oats.(22)
Also, different prebiotic sources, whether from supplements or foods, could be symptom triggering with some gut imbalances. Many prebiotic foods are considered fermentable FODMAP foods, thus they can contribute to symptoms and may be contraindicated in certain people for a period of time.(23) This can be the case in people that have small intestinal bacterial overgrowth (SIBO) for example.
This is why testing to see what’s in there first is always a good idea.
Why we start with food
You can’t out supplement a diet lacking in the first place. Food, barring food allergies and/or sensitivities, is a safe way to introduce nutrients, including probiotics (and prebiotics).
Some people however do struggle with histamine issues, in which case fermented foods might be triggering (this includes foods typically recommended for gut healing like bone broth, kefir, and sauerkraut).
However, even in my clients with histamine issues, there is a threshold (usually) so raw fermented foods like sauerkraut can be ok.
Certain probiotic supplements can increase histamine too (more on this below).
I find that typically in those with histamine sensitivities, it’s due to gut bug imbalances because certain bacteria produce histamine, and others degrade it. When we resolve gut imbalances, histamine can become a non-issue.
What to do/use if pregnant and/or nursing
Based on the research for eczema, supplementing mom with Bifidobacterium breve M-16V and Bifidobacterium longum BB536 during pregnancy, and mom and baby during the first 18 months of life may lower the incidence of eczema.(6,7)
L. rhamnosus supplementation for mom during pregnancy may lower chances of the baby developing eczema for the first 11 years of life, and may protect children from developing other atopic conditions like asthma, hay fever, and allergies.(8)
Why we need to test
Preferably even before starting a probiotic (because no supplement is benign) we test. Depending on what's happening in the gut, the wrong probiotic can make things worse by contributing to overgrowth for example, or by increasing histamine levels.
Gut bacteria, Histamine, and Probiotics
Gut bacteria might be contributing to your histamine-related symptoms, or might even be the root cause of them!
Bacteria play a role in producing and breaking down histamine. This ability is strain-specific and doesn’t apply to all strains within a species(29,30). Many probiotics purchased over the counter contain strains of bacteria that make histamine(29,30). This is why I’ve seen some clients’ symptoms worsen when they start taking a probiotic that is wrong for what’s happening with them.
Stop guessing which probiotic to use, get my FREE Guide “The probiotic mistake you’re making that’s flaring your child’s rashes” to find out which probiotics to avoid, and which to try instead.
Because bacteria play such a prominent role in histamine levels in the body, resolving imbalances in gut bacteria can address the root cause of histamine intolerance.
Why too much of a good thing is not a good thing
Excessive intake of probiotics can cause overgrowths/dysbiosis. I’ve had clients excessively consume probiotic foods and supplements, and induce gut symptoms and problems.
References
1. Kim J, Kim H. Microbiome of the Skin and Gut in Atopic Dermatitis (AD): Understanding the Pathophysiology and Finding Novel Management Strategies. J Clin Med. 2019;8(4):444. doi:10.3390/jcm8040444
2. Salem I, Ramser A, Isham N, Ghannoum MA. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front Microbiol. 2018;9:1459. doi:10.3389/fmicb.2018.01459
3. Arck P, Handjiski B, Hagen E, et al. Is there a ‘gut-brain-skin axis’? Exp Dermatol. 2010;19(5):401-405. doi:10.1111/j.1600-0625.2009.01060.x
4. Hill C, Guarner F, Reid G, et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506-514. doi:10.1038/nrgastro.2014.66
5. Rather IA, Bajpai VK, Kumar S, Lim J, Paek WK, Park Y-H. Probiotics and Atopic Dermatitis: An Overview. Front Microbiol. 2016;7. doi:10.3389/fmicb.2016.00507
6. Rautava S, Kainonen E, Salminen S, Isolauri E. Maternal probiotic supplementation during pregnancy and breast-feeding reduces the risk of eczema in the infant. J Allergy Clin Immunol. 2012;130(6):1355-1360. doi:10.1016/j.jaci.2012.09.003
7. Enomoto T, Sowa M, Nishimori K, et al. Effects of Bifidobacterial Supplementation to Pregnant Women and Infants in the Prevention of Allergy Development in Infants and on Fecal Microbiota. Allergol Int. 2014;63(4):575-585. doi:10.2332/allergolint.13-OA-0683
8. Wickens K, Barthow C, Mitchell EA, et al. Effects of Lactobacillus rhamnosus HN001 in early life on the cumulative prevalence of allergic disease to 11 years. Pediatr Allergy Immunol. 2018;29(8):808-814. doi:10.1111/pai.12982
9. Chen Y-H, Wu C-S, Chao Y-H, et al. Lactobacillus pentosus GMNL-77 inhibits skin lesions in imiquimod-induced psoriasis-like mice. J Food Drug Anal. 2017;25(3):559-566. doi:10.1016/j.jfda.2016.06.003
10. Groeger D, O’Mahony L, Murphy EF, et al. Bifidobacterium infantis 35624 modulates host inflammatory processes beyond the gut. Gut Microbes. 2013;4(4):325-339. doi:10.4161/gmic.25487
11. Vijayashankar M, Raghunath N. Pustular psoriasis responding to Probiotics – a new insight. Our Dermatol Online. 2012;3(4):326-329. doi:10.7241/ourd.20124.71
12. Marchetti F, Capizzi R, Tulli A. [Efficacy of regulators of the intestinal bacterial flora in the therapy of acne vulgaris]. Clin Ter. 1987;122(5):339-343.
13. Jung GW, Tse JE, Guiha I, Rao J. Prospective, Randomized, Open-Label Trial Comparing the Safety, Efficacy, and Tolerability of an Acne Treatment Regimen with and without a Probiotic Supplement and Minocycline in Subjects with Mild to Moderate Acne. J Cutan Med Surg. 2013;17(2):114-122. doi:10.2310/7750.2012.12026
14. Weiss E, Katta R. Diet and rosacea: the role of dietary change in the management of rosacea. Dermatol Pract Concept. 2017;7(4):31-37. doi:10.5826/dpc.0704a08
15. Scourboutakos MJ, Franco-Arellano B, Murphy SA, Norsen S, Comelli EM, L’Abbé MR. Mismatch between Probiotic Benefits in Trials versus Food Products. Nutrients. 2017;9(4). doi:10.3390/nu9040400
16. Tuohy KM, Brown DT, Klinder A, Costabile A, Fava F. Chapter 5 - Shaping the Human Microbiome with Prebiotic Foods – Current Perspectives for Continued Development**This is an update of: “Shaping the human microbiome with prebiotic foods – current perspectives for continued development.” Food Science and Technology Bulletin 2010; 7(4): 49–64. Available from: http://dx.doi.org/10.1616/1476-2137.15989 handle: http://hdl.handle.net/10449/19776. Re-published with the permission of International Food Information Service (IFIS Publishing). In: Tuohy K, Del Rio D, eds. Diet-Microbe Interactions in the Gut. Academic Press; 2015:53-71. doi:10.1016/B978-0-12-407825-3.00005-8
17. Rusu E, Enache G, Cursaru R, et al. Prebiotics and probiotics in atopic dermatitis (Review). Exp Ther Med. Published online June 14, 2019. doi:10.3892/etm.2019.7678
18. Spritzler F. What to know about inulin 101, a powerful prebiotic. Medical News Today. Published August 1, 2017. Accessed April 22, 2020. https://www.medicalnewstoday.com/articles/318593
19. Larch Arabinogalactan. WebMD. Accessed April 22, 2020. https://www.webmd.com/vitamins/ai/ingredientmono-974/larch-arabinogalactan
20. Mudgil D, Barak S, Patel A, Shah N. Partially hydrolyzed guar gum as a potential prebiotic source. Int J Biol Macromol. 2018;112:207-210. doi:10.1016/j.ijbiomac.2018.01.164
21. Chen K, Xie K, Liu Z, et al. Preventive Effects and Mechanisms of Garlic on Dyslipidemia and Gut Microbiome Dysbiosis. Nutrients. 2019;11(6):1225. doi:10.3390/nu11061225
22. What prebiotic foods should people eat? Medical News Today. Published October 1, 2018. Accessed April 22, 2020. https://www.medicalnewstoday.com/articles/323214
23. Sloan TJ, Jalanka J, Major GAD, et al. A low FODMAP diet is associated with changes in the microbiota and reduction in breath hydrogen but not colonic volume in healthy subjects. Green J, ed. PLOS ONE. 2018;13(7):e0201410. doi:10.1371/journal.pone.0201410
24. Tung JM, Dolovich LR, Lee CH. Prevention of Clostridium difficile Infection with Saccharomyces boulardii : A Systematic Review. Can J Gastroenterol. 2009;23(12):817-821. doi:10.1155/2009/915847
25. Namkin K, Zardast M, Basirinejad F. Saccharomyces Boulardii in Helicobacter Pylori Eradication in Children: A Randomized Trial From Iran. Iran J Pediatr. 2016;26(1). doi:10.5812/ijp.3768
26. Vitetta L, Saltzman E, Nikov T, Ibrahim I, Hall S. Modulating the Gut Micro-Environment in the Treatment of Intestinal Parasites. J Clin Med. 2016;5(11):102. doi:10.3390/jcm5110102
27. Stier H, Bischoff S. Influence of Saccharomyces boulardii CNCM I-745 on the gut-associated immune system. Clin Exp Gastroenterol. 2016;Volume 9:269-279. doi:10.2147/CEG.S111003
28. McFarlin BK, Henning AL, Bowman EM, Gary MA, Carbajal KM. Oral spore-based probiotic supplementation was associated with reduced incidence of post-prandial dietary endotoxin, triglycerides, and disease risk biomarkers. World J Gastrointest Pathophysiol. 2017;8(3):117. doi:10.4291/wjgp.v8.i3.117
29. Tee A. Probiotics for Histamine Intolerance: What You Need to Know. Available from https://factvsfitness.com/probiotics-histamine-intolerance/. Accessed June 1, 2021.
30. Ahmed S. Which probiotics for histamine intolerance? November 29, 2018. Available from https://www.optibacprobiotics.com/professionals/latest-research/general-health/which-probiotic-for-histamine-intolerance#:~:text=Certain%20types%20of%20bacteria%20can,no%20direct%20effect%20on%20histamine.&text=The%20ability%20to%20produce%20or,all%20strains%20within%20one%20species. Accessed June 1, 2021.