Photo Credit: WebMD, LLC
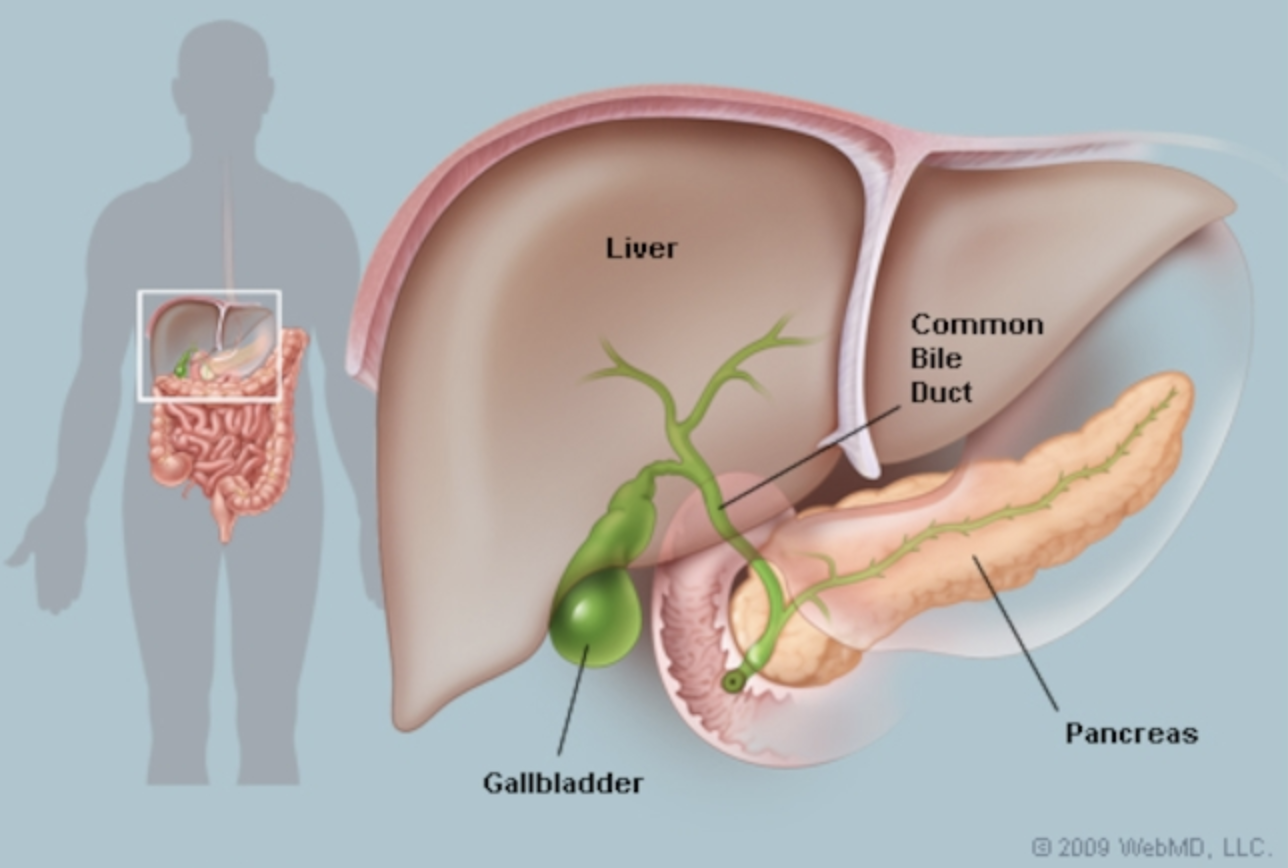
Bile and your gallbladder
You need fat in your diet for a wide range of reasons. Without dietary fat, you cannot absorb important fat-soluble nutrients including vitamins A, D, E, and K. Dietary fat provides energy, is required for hormone production, and your cell membranes are made up of fats (including your skin cells).
Bile is made in your liver and then it is stored in your gallbladder. Bile is released from your gallbladder during digestion. Bile allows your body digest and absorb fat.
Gallstones
When the concentration of a normal component of bile gets too high, gallstones can result. Bile is mainly made up of cholesterol, bile salts and phospholipids. Most gallstones (80% in the U.S.) are made of mixed components (usually cholesterol, bile salts, bile pigments, and inorganic salts of calcium).
Cholesterol stones are most common in women and in those living in larger bodies, and result from bile that is supersaturated with cholesterol.
Pigment stones can be black or brown, and they form when there is a lack of motility, or when there is excess unconjugated bilirubin.
If you have gallstones, finding out what kind is helpful because depending on what they are made of, there are different interventions that can be helpful.
Whatever the type, gallstones form when bile hardens into pieces. This requires three factors:
Bile must be supersaturated with cholesterol
Excess cholesterol with normal quantities of bile salts
Normal levels of cholesterol with decreased quantities of bile salts
Accelerated cholesterol crystal formation, or quick transition from liquid to crystal
High levels of factors (such as excess mucin) that form crystals
Lack of factors that inhibit crystal formation (dietary fish oils may inhibit crystal formation)
Low gallbladder motility
Crystals remain in the gallbladder too long and stones form
Some drugs can cause low motility
Low intestinal motility
Causes and risk factors for gallstones
Functional (examples)
Impaired liver transport of bile acids
Impaired secretion of bile acids
Low gallbladder and/or intestinal motility
Diet
Low fiber
High sugar
Coffee
High calorie
Rapid weight loss, and fasting
Food allergies/sensitivities can cause and contribute to gallbladder attacks. Common food triggers include:
Eggs
Pork
Onion
Turkey and chicken
Citrus (oranges, grapefruit)
Corn
Beans
Nuts and peanuts
Tomatoes
Soy
Gluten (wheat, barley, rye, other grains)
Dairy
Shellfish and fish
Metabolic imbalances
Obesity
Type 2 diabetes
Insulin resistance
Elevated blood triglycerides
Gender and hormones
Women are 2-4 times more likely to develop gallstones, and this may be due to increased cholesterol synthesis or suppression of bile acids by estrogens
Elevated estrogen levels (in men and women)
Hormone imbalances
Race
Gallbladder problems are more common in Native American women, likely due to diet and lifestyle factors
GI diseases
Crohn’s
Cystic fibrosis
Malabsorption of bile acids
Age
Average onset is 40-50 years old
With increased age, there is a natural decline in the activity of enzymes that make bile acids and this leads to increased cholesterol availability for the formation of gallstones (not necessarily due to high cholesterol levels)
Medications
Tamoxifen (breast cancer)
Oral contraceptives (birth control pills)
Ceftriaxone (antibiotic)
Octreotide (cancer treatment)
Statins and other lipid lowering drugs (cholesterol is needed to make bile acids)
Gallstones can be prevented with diet and lifestyle interventions
Maintain a healthy body weight
Avoid rapid weight loss and fad diets
An anti-inflammatory diet is recommended (Mediterranean style diet for example)
Lower intake of estrogenic foods (like soy)
Eliminate processed foods and sugar
Reduce intake of trans fats and fried foods
Increase fiber intake (especially soluble from flaxseed, oat bran, pectin, buckwheat)
Eat beets, artichoke and dandelion greens (they support digestive health because they improve bile flow to help break down fat)
Drink lots of water, at least 8 glasses per day
Easily digestible fats, consume in small amounts throughout the day (1-2 Tbsp at a time)
Fish oil
Coconut oil
Olive oil
Nutrients important for gallbladder health and support
Vitamin C: Bell peppers, papaya, citrus fruits, Brussels sprouts, strawberries, kiwi
Vitamin E: Sunflower seeds, spinach, Swiss chard, avocados, turnip greens, asparagus, mustard greens
Vitamin D: Salmon, herring and sardines, cod liver oil, canned light tuna (lower in mercury), oysters, egg yolk, mushrooms
Omega 3s/essential fatty acids: Flaxseed, eggs, fatty fish like salmon and fish oils (EPA and DHA), sea vegetables/seaweeds, avocado, coconut oil
Grape seed extract: Supplements
SAMe: Supplements
Phosphatidylcholine (made from choline): Eggs, liver, meat, poultry, fish and shellfish, dairy foods, rice, spinach, beets, supplements
Strict vegetarians and vegans who consume no meat, dairy, or eggs, can be at risk for inadequate choline intake
Other supplements for gallbladder support are available and should be customized for the needs of your body, to learn more about what is right for you, contact me
Gallbladder removal (cholecystectomy)
A cholecystectomy is most often performed to treat gallstones and the complications they cause. Your doctor may recommend this procedure if you have:
Gallstones
Gallbladder inflammation
Pancreas inflammation due to gallstones
It is important to remember that you need your gallbladder (no matter what your doctor says to the contrary) in order digest and absorb fats. It is essential for proper digestion!
If your gallbladder is removed you absolutely need to supplement with bile to make sure your body functions appropriately.
When you don’t have a gallbladder, diet changes can help, but will not replace or do away with the need to supplement bile. There are different bile supplements, and combination bile, stomach acid and enzyme products available. Your supplement needs to be customized for your body’s needs. To learn more about what is right for you, contact me.
References
Murray MT, Pizzorno J. Gallstones. The Encyclopedia of Natural Medicine, Third Edition. New York, NY: Atria; 2012. 605:614.
https://www.ncbi.nlm.nih.gov/pubmed/7652688
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3899548/
https://www.ncbi.nlm.nih.gov/pubmed/7719416
https://www.mayoclinic.org/tests-procedures/cholecystectomy/about/pac-20384818